As the world manages through the coronavirus pandemic, Arizona State University continues its work to discover and develop easier and more widespread COVID-19 testing to assist in managing the virus.
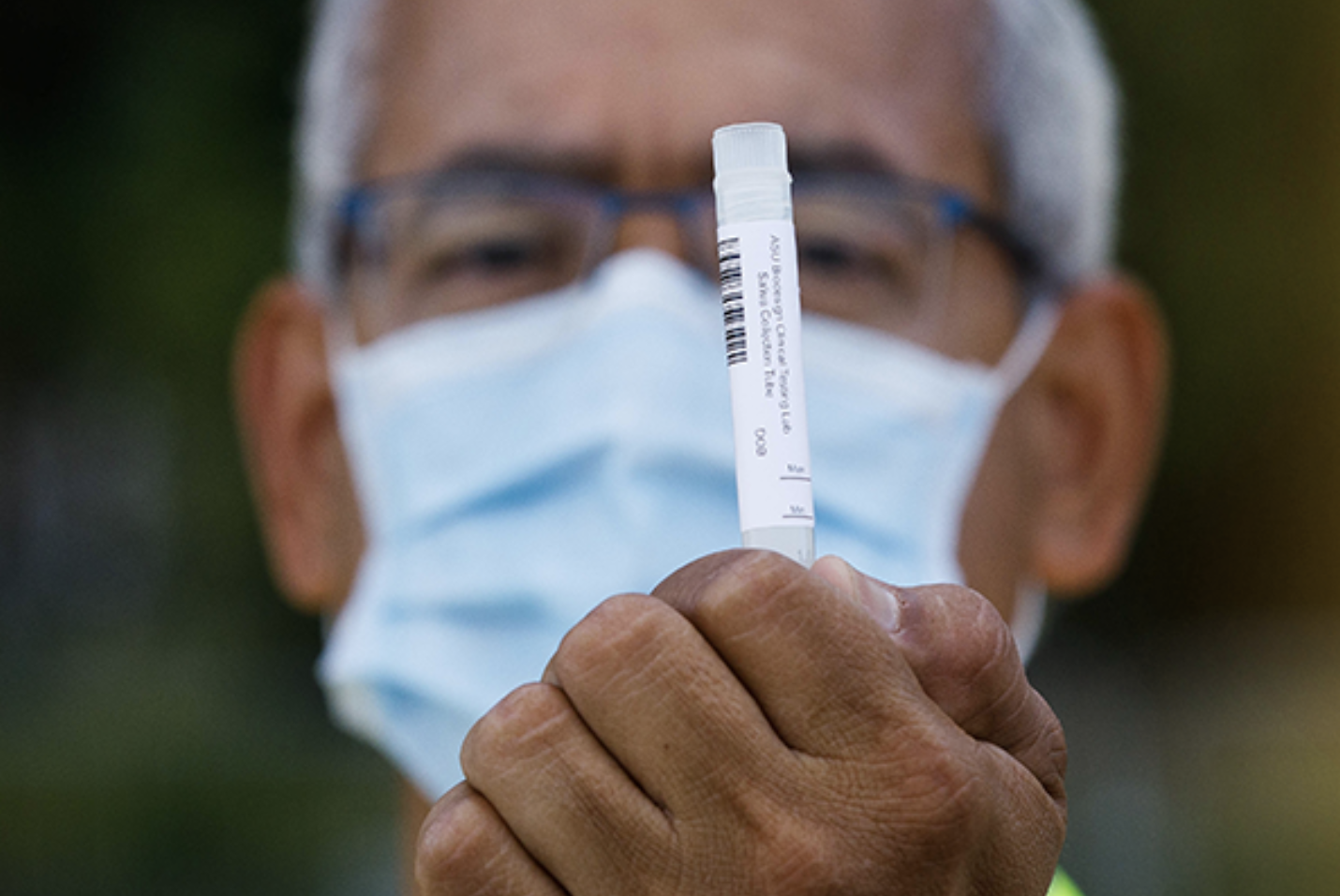
In May, researchers at ASU’s Biodesign Institute produced the Western United States’ first FDA-approved saliva-based COVID-19 test — one of only a handful available in the country — with test results delivered in 24–48 hours. Now, researchers are taking that work to the next level by building a new, portable saliva-based testing device that will deliver results in as little as 20 minutes.
Also referred to as a point-of-need test, users will be able to easily provide a saliva sample on a computer chip that will quickly detect whether the virus is present. The project is being funded by $5.2 million in CARES Act dollars from the governor’s office and $860,000 from the Arizona Department of Health Services. The CARES Act was passed by Congress in March to support coronavirus relief, research and response efforts.
“Arizona State University continues to lead the way in developing new technologies to help us respond to COVID-19 and protect Arizona communities,” said Gov. Doug Ducey. “We’re excited to work with our university partners on expanding access to COVID-19 testing, including investing in ASU’s groundbreaking point-of-need test. I’m grateful to President Crow and everyone at ASU for their commitment to finding creative solutions in the fight against COVID-19.”
Six months ago, ASU pivoted one of its research labs at the Biodesign Institute into a Clinical Laboratory Improvement Amendments (CLIA)-approved testing laboratory. The university began COVID-19 testing for front-line health care workers, critical infrastructure and public safety personnel. With a $12 million investment from Ducey in July, the university was able to quickly scale and deploy testing sites across the state with tests available to the public at no cost. To date, more than 36,000 Arizonans have received testing free of charge through the ASU/state of Arizona partner testing sites, a portion of the more than 135,000 tests ASU has run in total.
Gov. Ducey pledged an additional $8 million of funds to support university testing efforts.
“We are of the view that this virus will be with us in some capacity for the foreseeable future; therefore, we need to develop the most sophisticated tools in order to help manage it,” said ASU President Michael M. Crow. “This work is emblematic of ASU’s mission — we’re here to help solve grand challenges for society and to be of service to the people of Arizona.”
ASU professors Mark Hayes, Jennifer Blain Christen and Alexander Green are leads on the new COVID-19 testing device.
The team sees the test’s impact on managing COVID-19 as threefold:
• Distributed testing that is rapidly, conveniently and inexpensively available to anyone that needs it, for example in neighborhood drop-in clinics.
• A means of rapidly scaling testing across the state.
• Flexible, rapid, convenient testing in workplaces or schools to ensure a safe environment .
“Ultimately, we want to produce something easy to use so anyone could ‘spit on a chip’ while waiting for results for a few minutes and then be cleared for everyday activities or events, or rapidly isolated or ID’d as infected,” said Hayes.
The team’s interdisciplinary approach to building their prototype draws on a diverse group of specialists, who combined their expertise to make a difference during the pandemic. Hayes, with the ASU School of Molecular Sciences, is an expert in using tiny, liquid samples called microfluidics for biological analysis. Green, also with the ASU School of Molecular Sciences and ASU’s Biodesign Institute, designs biological sensors for detecting pathogens. Christen, of the Ira A. Fulton Schools of Engineering, develops handheld systems for thermal control and rapid optical readout of results.
The new rapid saliva test detects the viral RNA and combines the ease of use and speed of the newly FDA-approved antigen tests with greater accuracy similar to PCR-based RNA tests. If the virus is detected, a strong, green fluorescent signal is generated on the device. Also, unlike the PCR method, which needs a few hours of time because of several steps performed at different temperature cycles, this device is being designed to have all of the reactions performed at the same temperature.
A key point of the project will be mobility. Researchers envision a “plug and play” cartridge system that could be used by the ASU Biodesign Institute saliva-testing robotics system or implemented by practitioners without needing extensive training. By keeping the device small and portable, it can be rapidly employed and scaled in case of a surge in infection and done so locally and in a distributed fashion.
The ultimate goal is to have these devices accessible in public places such as doctors’ offices, workplaces and other densely populated areas. Through early detection, preventative measures can minimize contact risk and ensure safe spaces. Christen said their goal is to “ensure that we are able to get the best detection possible … while making sure it is financially accessible.”
Although the project is expected to generate working prototypes in six months and apply for FDA emergency-use authorization approval for COVID-19 testing, the team has already worked to align their technology with several companies for scalable production.